Anatomical sites 2
The peritoneum takes its innervation from the vagus nerve. It may be incompletely anaesthetized under spinal anaesthesia, and so its manipulation may cause discomfort. For this reason, spinal anaesthesia is not well suited to abdominal operations, other than those on the lower abdomen and/or abdominal wall.
Operations on the abdominal organs are rarely carried out under spinal anaesthesia, as peritoneal stimulation leads to an unacceptably high incidence of discomfort or pain.
A rarely used alternative to the single shot spinal or combined spinal-epidural (CSE), is the placement of an indwelling spinal catheter into the subarachnoid space. This means that small incremental spinal doses can be given, establishing the block gradually and in a controlled fashion. Further doses can be given to extend the duration of block. The catheter used is of extremely fine gauge to minimise post dural puncture headache. However, CSE can usually achieve an equivalent clinical result with equal safety, and without leaving a potential route for pathogens to directly reach the subarachnoid space.
Hence, the spinal catheter is usually reserved for the sickest patients (e.g. the very frail or those with severe fixed cardiac output disorder), where a dense block with precisely controllable onset is required. Because of this, and because of the intricacy of the technique, it is one for experienced practitioners only. It can, however, facilitate surgery in patients for whom other anaesthetic techniques are not an option.
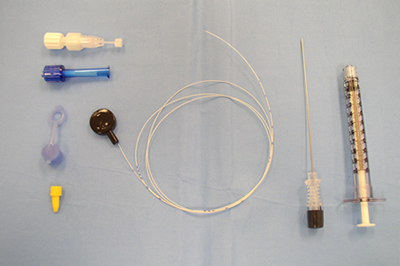
This is an example of a spinal microcatheter. This model employs a catheter (28 gauge) through needle (22 gauge) technique. A 1 ml syringe is required to generate enough fluid pressure to inject through the tiny catheter